The escalating challenge of antibiotic resistance in bacteria presents a grave threat to global health, impacting the efficacy of treatments for infectious diseases. With drug-resistant pathogens on the rise, many fear facing a future where once-treatable infections could become deadly. Understanding this pressing issue is not just for medical professionals; it is critical for everyone. The adverse effects of antibiotic resistance transcend borders, affecting families, communities, and health systems alike. As we delve deeper into this complex phenomenon, we will uncover the key drivers behind antibiotic resistance and explore potential pathways to combat this growing crisis.
The Escalating Threat of Antibiotic Resistance in Pathogens
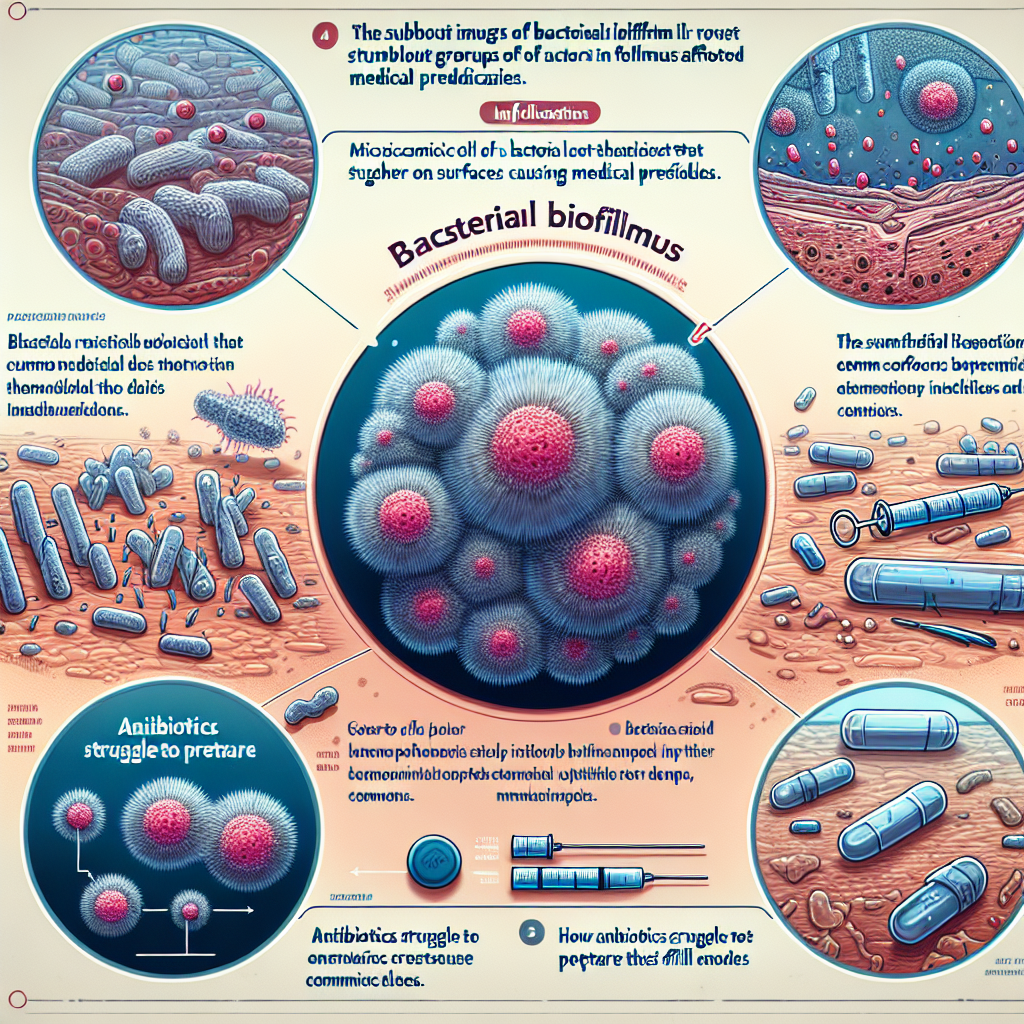
The emergence of antibiotic resistance in bacteria has reached alarming levels, rendering many common infections increasingly difficult to treat. Pathogens like Methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant Gram-negative bacteria are prime examples of this growing menace. These resistant strains can lead to prolonged illness, increased healthcare costs, and higher mortality rates. The World Health Organization (WHO) has highlighted that antibiotic resistance is one of the top ten global public health threats facing humanity, emphasizing the urgency of addressing this crisis.
Moreover, the implications of antibiotic resistance extend beyond individual health. When patients encounter infections that cannot be effectively treated, they may require more intensive care, longer hospital stays, and the use of more toxic or expensive alternative therapies. This not only strains healthcare resources but also poses a significant threat to surgical procedures and cancer treatments, which rely heavily on effective antibiotics to prevent postoperative infections. The increased burden on healthcare systems may lead to a ripple effect, undermining the efficiency of medical facilities and potentially leading to a public health disaster.
The rise in antibiotic resistance is particularly concerning because it renders many medical advances and treatments less effective. The prospect of returning to a pre-antibiotic era—where minor infections could once again become fatal—is not just fearmongering; it’s a reality that is inching closer. As our understanding of the mechanisms and factors driving antibiotic resistance deepens, it becomes crucial for healthcare professionals, policymakers, and the public to come together to devise comprehensive strategies that can effectively turn the tide on this formidable threat.
Key Factors Driving the Surge in Resistant Bacterial Strains
A myriad of factors contribute to the surge of resistant bacterial strains, with overprescribing and misuse of antibiotics at the forefront. In both human medicine and agriculture, the overutilization of antibiotics has created a perfect breeding ground for resistance. When antibiotics are prescribed without a clear indication or when patients fail to complete their courses, the surviving bacteria adapt, often becoming resistant to that particular drug. This misuse not only impacts individual patients but also has wider implications for public health.
Another significant contributor to the rise of antibiotic resistance is the alarming trend of antibiotic use in livestock production. The routine use of antibiotics in agriculture—often for growth promotion or disease prevention—has been a controversial practice that fosters the emergence of resistant bacteria. These resistant strains can then be transmitted to humans through the food chain or environmental contamination, complicating the already challenging landscape of antibiotic resistance. This interplay between human health and agricultural practices underscores the urgent need for a holistic approach to managing antibiotic use across sectors.
Furthermore, the lack of new antibiotic development contributes to the growing challenge. Pharmaceutical companies face significant barriers in developing novel antibiotics, including high research and development costs and modest financial incentives. As existing drugs become ineffective, the dwindling pipeline of new antibiotics exacerbates the crisis. This situation calls for innovative approaches to stimulate antibiotic research and development, alongside promoting stewardship programs that encourage responsible antibiotic use in both healthcare and agricultural settings.
As we confront the growing challenge of antibiotic resistance in bacteria, a multifaceted approach is essential for curbing this escalating threat. By understanding the factors contributing to resistance and advocating for responsible antibiotic use, we can help protect the efficacy of these critical drugs. The conversation around antibiotic resistance must continue to evolve, engaging not just healthcare providers but also patients and policymakers. Now is the time to take action, whether through education, advocacy, or support for research initiatives aimed at combating this pressing issue. Together, we can forge a path toward a healthier future, ensuring that effective treatments remain available for generations to come.
Essential Strategies for Preventing Viral Infections EffectivelyEssential Strategies for Preventing Bacterial InfectionsUnderstanding the Mechanisms of Virus and Bacteria TransmissionRelevant LinkRelevant LinkRelevant LinkUnderstanding Lower Back Pain Linked to COVID-19: Insights and ManagementUnderstanding COVID-19: Navigating Loss of Appetite ChallengesUnderstanding COVID Laryngitis: Symptoms, Causes, and TreatmentRelevant LinkRelevant LinkRelevant Link