Bacterial biofilms pose a significant threat to health by complicating infection management and treatment strategies. These complex communities of microorganisms can form on various surfaces within the human body, creating a protective environment that shields them from both the immune system and antimicrobial therapies. Understanding bacterial biofilms is crucial for healthcare professionals, as their implications extend deeply into chronic infections, medical device failures, and surgical outcomes. This article will explore the intricacies of bacterial biofilms and their substantial consequences on health, providing valuable insights for better infection management and treatment approaches.
Understanding the Formation and Structure of Bacterial Biofilms
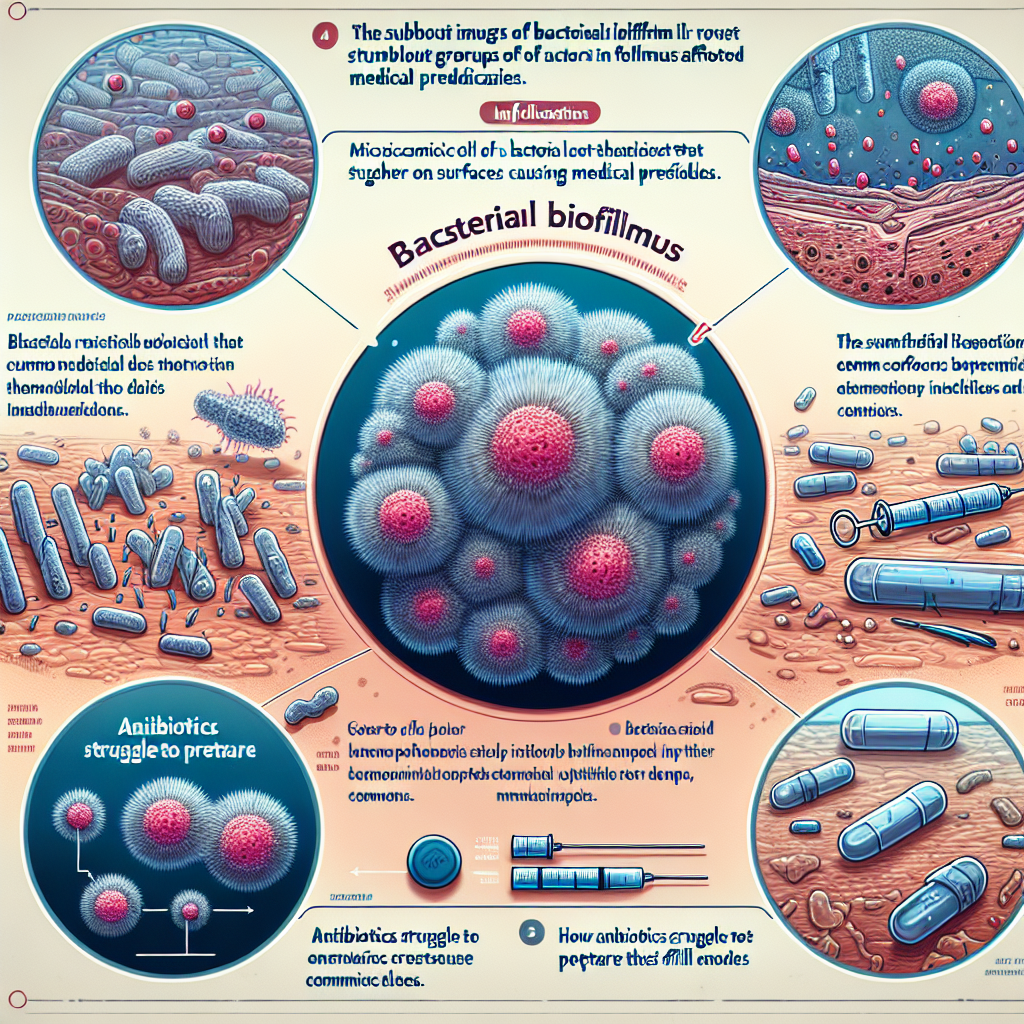
Bacterial biofilms are structured communities of microorganisms that adhere to surfaces, encapsulated in a self-produced extracellular polymeric substance (EPS). This matrix provides structural stability and protection, allowing biofilms to thrive in hostile environments. The formation of biofilms begins with the attachment of free-floating bacteria to a surface, followed by cell division and the production of EPS, which facilitates the clustering of additional bacterial cells. Over time, these clusters evolve into complex, layered structures that can vary significantly in thickness and density, depending on the species involved and environmental conditions.
The composition of biofilms is diverse, often involving multiple species of bacteria, fungi, and even protozoa. This diversity not only enhances the resilience of biofilms but also complicates the treatment of infections they cause. The intricate architecture of biofilms can create microenvironments with different nutrient and oxygen levels, enabling various microorganisms to coexist and thrive. This dynamic interplay among species fosters a unique ecological niche that is challenging to penetrate with conventional treatments, leading to chronic infections and persistent health issues.
Biofilms can develop on a multitude of surfaces in the human body, including teeth, medical devices, and within tissues. Understanding the environmental conditions that favor biofilm formation is essential for anticipating and mitigating their impacts. Factors such as low nutrient availability, surface roughness, and fluid flow rates can significantly influence biofilm development. By exploring these factors, healthcare professionals can begin to devise strategies to prevent and disrupt biofilm formation, ultimately improving patient outcomes.
The Impact of Biofilms on Infection Management and Treatment
The presence of bacterial biofilms has profound implications for infection management and treatment, complicating the healing process and leading to persistent health challenges. Biofilms are notoriously resistant to antibiotics, making traditional treatments often ineffective. The EPS matrix protects the microorganisms from antimicrobial agents, while the slow-growing cells within biofilms exhibit a dormancy that contributes to their resilience. This resistance frequently results in prolonged infection duration, increased healthcare costs, and a higher burden of morbidity for patients.
Moreover, biofilms are associated with various medical conditions, including chronic wounds, otitis media, and catheter-associated urinary tract infections. The persistence of these infections can lead to significant complications, including systemic infections and increased morbidity. In the case of medical devices, biofilm formation can lead to device failure, necessitating replacement surgeries that are not only costly but also expose patients to additional risks. The struggle against biofilm-associated infections represents a significant challenge for healthcare providers, highlighting the need for innovative treatment approaches.
Emerging strategies to combat bacterial biofilms include the development of novel antimicrobial agents and therapies aimed at disrupting biofilm structure. For instance, the use of enzymes capable of degrading EPS, as well as the incorporation of anti-biofilm coatings on medical devices, shows promise in reducing biofilm-related complications. Additionally, pharmacological agents that target bacterial communication, known as quorum sensing, are being investigated as a means to impede biofilm formation and promote the efficacy of existing antibiotics. These cutting-edge approaches could revolutionize how healthcare practitioners manage biofilm-related infections and significantly improve patient outcomes.
The intricate relationship between bacterial biofilms and health underscores the importance of understanding these microbial communities in medical practice. Their formation, structure, and persistent nature pose challenges that can lead to severe health complications, highlighting the need for continued research and innovative treatment strategies. By keeping abreast of the latest developments in biofilm management, healthcare professionals can better navigate the complexities of infection control and improve patient care. Engaging in ongoing education and exploring novel approaches can empower practitioners to effectively combat the impact of bacterial biofilms, ultimately leading to a new era of infection management in medicine. For those looking to delve deeper into this topic, further exploration of advanced treatment options and preventive measures is highly encouraged.
Essential Strategies for Preventing Viral Infections EffectivelyEssential Strategies for Preventing Bacterial InfectionsUnderstanding the Mechanisms of Virus and Bacteria TransmissionRelevant LinkRelevant LinkRelevant LinkUnderstanding Lower Back Pain Linked to COVID-19: Insights and ManagementUnderstanding COVID-19: Navigating Loss of Appetite ChallengesUnderstanding COVID Laryngitis: Symptoms, Causes, and TreatmentRelevant LinkRelevant LinkRelevant Link